Understanding bladder health requires acknowledging potential complications like calcification in bladder wall, a condition where calcium deposits form within the bladder’s structure. Diagnostic imaging, such as a CT scan, plays a crucial role in identifying the extent and location of these deposits. Medical research at institutions like the Mayo Clinic contributes significantly to our understanding of the underlying mechanisms driving this process. Furthermore, consultation with a urologist is essential for proper diagnosis and management of patients presenting with symptoms related to calcification in bladder wall.
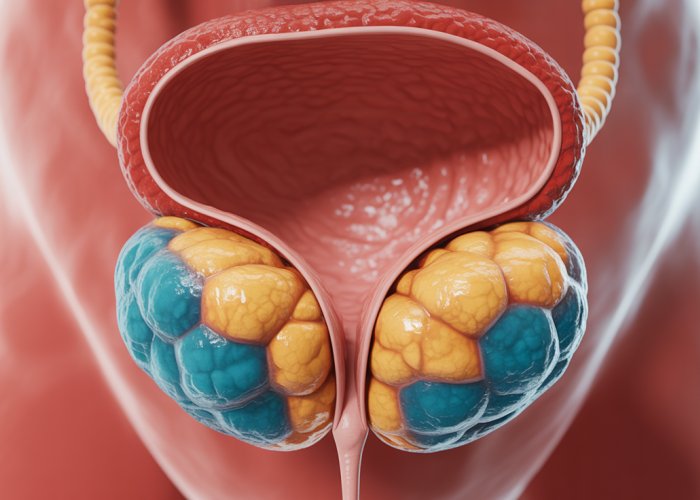
The bladder, a vital organ within the human body, acts as a reservoir for urine, facilitating its storage and controlled release. Understanding its normal function is paramount to appreciating the significance of pathological conditions that can arise, such as bladder wall calcification.
The Bladder: A Reservoir of Life
The bladder’s primary function is to collect and store urine, a waste product generated by the kidneys. This process allows for the intermittent elimination of urine, preventing constant leakage and enabling social continence. The bladder’s walls are composed of layers of smooth muscle that expand to accommodate varying volumes of urine and contract during urination.
Calcification: A Hard Truth
Calcification, in its simplest terms, refers to the deposition of calcium salts within body tissues. While calcification is a natural and necessary process in bone formation, its occurrence in soft tissues like the bladder wall is invariably abnormal and indicative of an underlying pathological process.
Bladder Wall Calcification: An Abnormal Transformation
Bladder wall calcification signifies the unnatural accumulation of calcium deposits within the bladder’s structure. This process can compromise the bladder’s elasticity and functionality, leading to a spectrum of clinical manifestations. It’s a condition that warrants thorough investigation and appropriate management.
Decoding the Phenomenon: Purpose of this Article
This article aims to serve as a comprehensive guide, providing a clear and concise explanation of bladder wall calcification. We intend to illuminate the underlying mechanisms, causes, diagnostic approaches, and potential treatment strategies associated with this medical phenomenon. Our goal is to empower readers with the knowledge needed to understand this condition and engage in informed discussions with healthcare professionals.
The previous section laid the groundwork by introducing bladder wall calcification as an abnormal process, highlighting its departure from the bladder’s normal, healthy state. Now, let’s delve deeper into the intricacies of this phenomenon, exploring the mechanisms behind its formation, the relevant anatomy, and the very stuff that these abnormal deposits are made of.
Understanding Bladder Wall Calcification: A Deep Dive
Bladder wall calcification isn’t just a simple accumulation of calcium; it’s a complex process with significant implications for bladder function. A comprehensive understanding requires exploring the specific mechanisms involved in calcium deposition, the anatomy of the bladder wall, and the composition of these unusual formations.
What is Bladder Wall Calcification?
At its core, bladder wall calcification involves the abnormal deposition of calcium salts within the tissues of the bladder wall.
This process is markedly different from normal calcification, such as that involved in bone formation, where it is a controlled and essential physiological process.
In the bladder, however, calcification signifies a pathological alteration of the tissue environment.
The Process of Calcium Deposition
The exact mechanisms that trigger calcium deposition in the bladder wall are varied and can be complex.
It often starts with tissue damage or inflammation.
This initial injury disrupts the local cellular environment.
This disruption then leads to the release of substances that promote the precipitation of calcium and phosphate ions.
These ions then bind together to form insoluble calcium salts.
Over time, these salts accumulate, forming deposits within the bladder wall.
Normal vs. Abnormal Calcification
It’s crucial to distinguish between physiological (normal) and pathological (abnormal) calcification.
Normal calcification is tightly regulated.
It occurs in specific locations, such as bones and teeth, and is essential for their structural integrity.
Abnormal calcification, on the other hand, occurs in soft tissues where it should not be present.
It’s usually a sign of an underlying problem.
It indicates tissue damage, inflammation, or metabolic imbalances.
In the bladder, calcification disrupts the normal function of the bladder wall, affecting its elasticity and ability to contract and relax properly.
Anatomy of the Bladder and Bladder Wall
To fully appreciate the impact of calcification, it’s essential to understand the anatomy of the bladder wall.
The bladder wall is composed of several distinct layers, each with a specific role in bladder function.
Layers of the Bladder Wall
The bladder wall primarily consists of three main layers:
- The mucosa: The innermost layer, lined with transitional epithelium (urothelium) designed to withstand the harsh chemical environment of urine.
- The muscularis propria (detrusor muscle): A thick layer of smooth muscle responsible for bladder contraction during urination.
- The serosa or adventitia: The outermost layer, composed of connective tissue that provides structural support and connects the bladder to surrounding tissues.
Impact of Calcification on Bladder Wall Layers
Calcification can affect any or all of these layers.
- Calcification in the mucosa can cause irritation and ulceration, leading to symptoms like pain and hematuria.
- Calcification within the muscularis propria can impair the bladder’s ability to contract effectively.
- Extensive calcification can reduce the bladder’s overall capacity and elasticity.
The location and extent of calcification directly impact the severity of symptoms and the choice of treatment strategies.
Composition of Calcification
The composition of bladder wall calcification is predominantly calcium phosphate.
It often presents in a crystalline form.
Understanding the composition of these deposits can offer clues about the underlying causes and potential treatment targets.
Calcium and Phosphate: The Main Ingredients
Calcium and phosphate are the primary components of these calcified deposits.
The ratio of calcium to phosphate can vary depending on the specific conditions within the bladder.
Other minerals, such as magnesium, may also be present in smaller amounts.
Crystalline Structure
The calcium phosphate often forms a crystalline structure.
Hydroxyapatite is the most common crystalline form found in bladder wall calcification.
The crystalline structure contributes to the hardness and insolubility of the deposits.
This makes them difficult for the body to naturally dissolve or remove.
The presence of these crystals further irritates the bladder tissue.
It also contributes to inflammation and damage.
The previous section laid the groundwork by introducing bladder wall calcification as an abnormal process, highlighting its departure from the bladder’s normal, healthy state. Now, let’s delve deeper into the intricacies of this phenomenon, exploring the mechanisms behind its formation, the relevant anatomy, and the very stuff that these abnormal deposits are made of.
Causes and Risk Factors: Pinpointing the Origins
Understanding the etiology of bladder wall calcification is crucial for effective prevention and management.
This condition arises from a variety of factors, some more prevalent than others, and certain predisposing conditions can significantly elevate an individual’s risk.
Let’s explore these origins, separating the common culprits from the less frequent ones, and identifying the key risk factors that contribute to the development of this condition.
Common Causes of Bladder Wall Calcification
Several factors are frequently implicated in the development of bladder wall calcification.
These often involve inflammatory processes or the presence of foreign materials within the bladder.
Urinary Tract Infections (UTIs) and Calcification
Urinary Tract Infections (UTIs) stand out as a significant instigator of bladder wall calcification.
The inflammatory response triggered by a UTI can damage the bladder lining.
This damage creates an environment conducive to calcium deposition.
Chronic or recurrent UTIs are particularly problematic, as the repeated cycles of inflammation and repair increase the likelihood of calcification over time.
The bacteria involved in UTIs can also directly influence the chemical environment in the bladder.
This influence promotes the precipitation of calcium salts.
Chronic Inflammation of the Bladder Wall
Beyond UTIs, any source of chronic inflammation in the bladder wall can contribute to calcification.
This inflammation, regardless of its origin, disrupts the normal cellular processes and can lead to tissue damage.
Damaged tissue is more susceptible to the deposition of calcium and phosphate ions, the building blocks of calcification.
Conditions like interstitial cystitis, a chronic bladder pain syndrome, can cause persistent inflammation.
This persistent inflammation elevates the risk of calcification.
Impact of Foreign Bodies in the Bladder
The presence of foreign bodies within the bladder can also trigger calcification.
These foreign bodies, such as forgotten surgical sutures or migrated objects, act as nidus points for calcium salt deposition.
The body’s natural response to these foreign objects involves inflammation and the deposition of proteins and other substances on their surface.
These substances can then attract calcium and phosphate ions, leading to the gradual formation of calcified deposits around the foreign body.
Less Common Causes of Bladder Wall Calcification
While UTIs, chronic inflammation, and foreign bodies are the most frequently encountered causes, other, less common factors can also contribute to bladder wall calcification.
Schistosomiasis and Bladder Calcification
Schistosomiasis, a parasitic disease prevalent in certain regions of the world, is a well-documented cause of bladder wall calcification.
The Schistosoma haematobium parasite, responsible for urinary schistosomiasis, resides in the blood vessels surrounding the bladder.
Over time, the eggs laid by these parasites can become embedded in the bladder wall, causing chronic inflammation and tissue damage.
This chronic inflammation and damage lead to calcification of the bladder wall.
Schistosomiasis-related calcification often presents with a characteristic pattern.
This pattern can be identified through imaging studies.
Association with Bladder Cancer
Although far less common, bladder wall calcification can sometimes be associated with bladder cancer.
In some instances, the presence of a tumor can disrupt the normal tissue environment.
This disruption promotes the deposition of calcium salts.
It’s important to emphasize that calcification does not necessarily indicate the presence of cancer.
However, when calcification is detected, it’s crucial to rule out malignancy through appropriate diagnostic procedures.
Risk Factors for Bladder Wall Calcification
Certain factors can increase an individual’s susceptibility to developing bladder wall calcification.
These risk factors can be broadly categorized as demographic, physiological, and environmental.
Age, Gender, and Predisposing Conditions
Age plays a role, as the likelihood of developing chronic conditions that contribute to calcification increases with age.
Gender can also be a factor, with some studies suggesting a higher prevalence in women, potentially due to the increased risk of UTIs.
Certain pre-existing conditions can also elevate the risk.
These conditions includes diabetes, which can impair immune function and increase the risk of infections, and conditions that predispose to urinary stasis, such as bladder outlet obstruction.
The previous section delved into the origins of bladder wall calcification, exploring the diverse factors that can trigger this abnormal process. Understanding what causes it sets the stage for recognizing the problem when it arises. This involves understanding the symptoms patients experience and the diagnostic tools available to confirm the presence and extent of calcification.
Symptoms and Diagnosis: Recognizing and Identifying the Problem
Recognizing the signs and symptoms of bladder wall calcification is the first step toward diagnosis and appropriate management. Because symptoms can be subtle or mimic other urological conditions, a thorough diagnostic workup is essential for accurate identification.
Symptoms of Bladder Wall Calcification
The symptoms associated with bladder wall calcification can vary greatly depending on the size, location, and extent of the calcification. Some individuals may experience no noticeable symptoms at all, particularly in the early stages. As the calcification progresses, however, several common symptoms may emerge.
-
Pain: Pain is a frequent complaint, often described as a persistent ache or discomfort in the lower abdomen or pelvic region. The pain may be constant or intermittent, and it can be exacerbated by urination.
-
Frequent Urination (Frequency): Calcification can irritate the bladder lining, leading to an increased urge to urinate. Patients may find themselves needing to urinate more frequently than usual, both during the day and at night (nocturia).
-
Hematuria (Blood in Urine): The presence of blood in the urine, known as hematuria, is another potential symptom. This can range from microscopic hematuria (detectable only under a microscope) to gross hematuria (visible to the naked eye). Hematuria often results from the calcification eroding the bladder lining.
-
Urgency: This is an uncontrollable need to urinate immediately.
-
Dysuria: This describes painful or difficult urination.
The severity and presentation of these symptoms can vary significantly from person to person. A small, localized area of calcification might produce minimal symptoms, while more extensive calcification affecting a larger portion of the bladder wall is more likely to cause pronounced symptoms.
It’s also important to note that the location of the calcification within the bladder can influence the specific symptoms experienced. Calcification near the bladder neck, for example, might contribute to urinary retention or difficulty initiating urination.
Diagnostic Procedures for Bladder Wall Calcification
A combination of imaging techniques, endoscopic evaluation, and tissue biopsy is typically employed to diagnose bladder wall calcification.
Imaging Techniques
Several imaging modalities play a crucial role in visualizing calcification within the bladder wall:
-
X-rays: Plain abdominal X-rays can sometimes detect calcification, particularly if the deposits are large and dense. However, X-rays are not always sensitive enough to identify smaller areas of calcification.
-
CT Scans (Computed Tomography): CT scans are far more sensitive than X-rays in detecting calcification. They provide detailed cross-sectional images of the bladder and surrounding structures, allowing for precise localization and assessment of the extent of calcification. CT scans are often the preferred imaging modality for evaluating bladder wall calcification.
-
Ultrasounds: Ultrasounds, while less sensitive than CT scans, can be useful in detecting calcification, particularly in patients who cannot undergo CT scanning (e.g., pregnant women).
Cystoscopy
Cystoscopy involves inserting a thin, flexible tube with a camera attached (cystoscope) into the bladder through the urethra. This allows for direct visualization of the bladder lining and identification of any abnormalities, including calcification.
Cystoscopy enables the urologist to directly inspect the bladder wall. It helps differentiate calcification from other potential bladder abnormalities, such as tumors or inflammation.
Biopsy
A biopsy involves taking a small tissue sample from the bladder wall for microscopic examination. A biopsy is often performed during cystoscopy if abnormalities are seen.
The tissue sample is sent to a pathologist, who examines it under a microscope to confirm the presence of calcification. The pathologist can also rule out other conditions, such as bladder cancer or inflammation, which may mimic calcification on imaging studies.
A biopsy is essential for definitive diagnosis, especially when other conditions need to be excluded.
The Roles of Radiologists and Pathologists
The diagnostic process for bladder wall calcification involves the expertise of several medical specialists. Radiologists play a key role in interpreting imaging studies, such as CT scans and X-rays, to identify areas of calcification. Pathologists analyze tissue samples obtained through biopsy to confirm the diagnosis and rule out other conditions.
The collaboration between radiologists, pathologists, and urologists ensures an accurate and comprehensive diagnosis of bladder wall calcification, which is crucial for determining the most appropriate treatment strategy.
The previous section delved into the origins of bladder wall calcification, exploring the diverse factors that can trigger this abnormal process. Understanding what causes it sets the stage for recognizing the problem when it arises. This involves understanding the symptoms patients experience and the diagnostic tools available to confirm the presence and extent of calcification.
Treatment Options: Addressing Bladder Wall Calcification
Once bladder wall calcification has been diagnosed, the next crucial step involves determining the most appropriate course of treatment. The optimal approach will depend on several factors, including the severity of the calcification, the presence of symptoms, the underlying cause, and the patient’s overall health. Treatment strategies range from conservative, non-surgical management to more invasive surgical interventions. Urologists play a central role in guiding this decision-making process and tailoring treatment plans to individual patient needs.
Non-Surgical Treatment Strategies
In many cases, particularly when calcification is minimal or asymptomatic, non-surgical approaches may be sufficient to manage the condition and alleviate any associated symptoms. These strategies primarily focus on addressing the underlying causes and providing symptomatic relief.
Medications for Symptom Management and Underlying Causes
Pharmacological interventions often form the cornerstone of non-surgical management. If a urinary tract infection (UTI) is identified as a contributing factor, a course of antibiotics will be prescribed to eradicate the infection and prevent further inflammation.
Analgesics, or pain relievers, can be used to manage discomfort or pain associated with calcification. In cases where bladder spasms contribute to the pain, antispasmodic medications may be beneficial.
Addressing underlying conditions, such as metabolic disorders that may contribute to calcium deposition, is also crucial.
Lifestyle Modifications
Certain lifestyle adjustments can also play a supportive role in managing bladder wall calcification. Adequate hydration is essential for maintaining optimal bladder function and reducing the concentration of minerals in the urine.
Dietary modifications, such as limiting calcium intake, may be recommended in some cases, although this is generally not the primary focus of treatment. Avoiding bladder irritants, such as caffeine and alcohol, can help to reduce urinary frequency and urgency.
Regular exercise and maintaining a healthy weight can also contribute to overall bladder health.
Surgical Treatment Options
When non-surgical approaches prove inadequate or when calcification is extensive and causing significant symptoms or complications, surgical intervention may be necessary. The primary goal of surgery is to remove the calcified areas and restore normal bladder function.
Surgical Removal of Calcified Areas
Surgical removal of calcified areas is typically reserved for severe cases where calcification is causing significant pain, obstruction, or other complications. There are several surgical approaches available, each with its own advantages and disadvantages.
Surgical Approaches: A Comparative Analysis
-
Transurethral Resection: This minimally invasive approach involves inserting a cystoscope (a thin, flexible tube with a camera) through the urethra to visualize the bladder. Using specialized instruments, the surgeon can then carefully remove the calcified areas. This approach avoids external incisions and typically results in a shorter recovery time.
-
Open Surgery: In some cases, particularly when calcification is extensive or complex, open surgery may be necessary. This involves making an incision in the lower abdomen to directly access the bladder and remove the calcified areas. While open surgery allows for more extensive access and removal of calcification, it also carries a higher risk of complications and a longer recovery period.
-
Laparoscopic Surgery: This minimally invasive technique uses small incisions and a camera to guide the surgeon in removing the calcified areas. Laparoscopic surgery offers advantages over open surgery, such as reduced pain, scarring, and recovery time.
The choice of surgical approach will depend on the individual patient’s circumstances, the extent and location of the calcification, and the surgeon’s expertise.
The Urologist’s Pivotal Role
Urologists are the medical specialists who are best equipped to diagnose and treat bladder wall calcification. They have extensive training and experience in managing a wide range of urological conditions, including bladder disorders.
Urologists play a critical role in:
- Diagnosis: Performing diagnostic tests, such as cystoscopy and imaging studies, to confirm the presence and extent of calcification.
- Treatment Planning: Developing individualized treatment plans based on the patient’s specific needs and circumstances.
- Surgical Intervention: Performing surgical procedures to remove calcified areas.
- Post-operative Care: Providing ongoing care and monitoring to ensure optimal outcomes and prevent recurrence.
Patients should seek consultation with a qualified urologist for accurate diagnosis, comprehensive treatment, and long-term management of bladder wall calcification.
The preceding sections have explored the identification and treatment of bladder wall calcification. But what happens if calcification is left unaddressed or improperly managed? Understanding the potential complications and the long-term outlook is crucial for both patients and healthcare providers. Let’s delve into what to expect regarding complications and prognosis.
Complications and Prognosis: What to Expect
Bladder wall calcification, while sometimes asymptomatic, can lead to a range of complications if left untreated. The prognosis, or expected outcome, varies depending on the severity, underlying cause, and timeliness of intervention. Early diagnosis and appropriate management are paramount in mitigating potential adverse effects and improving long-term outcomes.
Potential Complications of Untreated Calcification
Ignoring bladder wall calcification can result in several concerning complications. These can significantly impact bladder function and overall quality of life.
Impaired Bladder Function
One of the most significant risks associated with untreated calcification is impaired bladder function. As calcium deposits accumulate within the bladder wall, the bladder’s ability to expand and contract effectively can be compromised.
This can lead to:
- Reduced bladder capacity, resulting in frequent urination.
- Urgency, or a sudden and compelling need to urinate.
- Incomplete emptying of the bladder, which can further contribute to infection risk.
In severe cases, the bladder may lose its elasticity, leading to urinary retention and potentially requiring catheterization.
Increased Risk of Infections
Calcification can create an environment conducive to bacterial growth, significantly increasing the risk of recurrent urinary tract infections (UTIs). The irregular surface of the calcified areas can act as a nidus for bacteria to adhere to, making it difficult for the bladder to completely clear the infection.
Chronic or recurrent UTIs can lead to further inflammation and damage to the bladder wall, perpetuating a vicious cycle of infection and calcification. In some instances, persistent infections may ascend to the kidneys, causing pyelonephritis, a more serious and potentially life-threatening condition.
Malignant Transformation: A Rare but Serious Concern
While relatively rare, there is a potential, albeit small, risk of malignant transformation associated with chronic bladder wall calcification. The persistent inflammation and cellular damage caused by calcification can, over time, contribute to the development of bladder cancer.
It’s important to emphasize that the vast majority of cases of bladder wall calcification do not lead to cancer. However, the possibility exists, underscoring the importance of regular monitoring and follow-up, especially in individuals with long-standing calcification or other risk factors for bladder cancer.
Prognosis and Long-Term Outlook
The prognosis for patients with bladder wall calcification is generally favorable, especially when the condition is diagnosed and treated promptly. The long-term outlook depends on several factors:
-
Severity of the Calcification: Mild calcification with minimal symptoms often has an excellent prognosis, particularly if the underlying cause is addressed.
-
Underlying Cause: Successfully treating the underlying cause, such as a chronic UTI or foreign body, can prevent further calcification and improve the overall prognosis.
-
Timeliness of Intervention: Early diagnosis and treatment are crucial to prevent complications and improve the long-term outlook.
-
Patient Compliance: Adhering to prescribed medications, lifestyle modifications, and follow-up appointments is essential for successful management and a positive prognosis.
The Importance of Early Diagnosis and Management
As highlighted throughout this section, early diagnosis and appropriate management are paramount in determining the prognosis for bladder wall calcification. Regular check-ups, prompt attention to urinary symptoms, and adherence to medical advice can significantly improve outcomes.
If you are experiencing symptoms such as pain, frequent urination, or blood in the urine, it is crucial to seek medical attention promptly. Early diagnosis and appropriate treatment can help prevent complications and ensure a better long-term outlook.
The preceding sections have explored the identification and treatment of bladder wall calcification. But what happens if calcification is left unaddressed or improperly managed? Understanding the potential complications and the long-term outlook is crucial for both patients and healthcare providers. Let’s delve into what to expect regarding complications and prognosis.
Prevention: Reducing Your Risk of Bladder Wall Calcification
While not always entirely preventable, adopting certain lifestyle measures and proactively managing underlying health conditions can significantly reduce the risk of developing bladder wall calcification. Prevention strategies primarily focus on minimizing factors that contribute to bladder inflammation and maintaining optimal urinary health. Let’s explore some key recommendations.
Lifestyle Adjustments for Bladder Health
Simple lifestyle modifications can profoundly impact bladder health and reduce the likelihood of calcification. These changes are often easy to implement and can contribute to overall well-being.
Adequate Hydration: The Cornerstone of Prevention
Drinking plenty of water is paramount for maintaining a healthy urinary tract. Increased fluid intake helps dilute urine, reducing the concentration of minerals that can contribute to calcification.
Aim for at least eight glasses of water per day, adjusting the amount based on activity level, climate, and individual health conditions. Proper hydration also aids in flushing out bacteria, thus lowering the risk of UTIs, a major contributor to bladder inflammation.
Dietary Considerations: Balancing Mineral Intake
While calcium is essential for overall health, excessive intake, particularly without adequate magnesium and vitamin D, can potentially contribute to calcification in susceptible individuals.
Consult with a healthcare professional or registered dietitian to ensure a balanced intake of essential minerals. They can help you optimize your diet for both overall health and bladder health.
Limiting processed foods, sugary drinks, and excessive salt intake can also contribute to a healthier urinary tract environment.
Regular Exercise: Promoting Circulation and Immune Function
Regular physical activity improves circulation, strengthens the immune system, and helps maintain a healthy weight, all of which can indirectly benefit bladder health.
Aim for at least 30 minutes of moderate-intensity exercise most days of the week. Even simple activities like walking, swimming, or cycling can make a significant difference.
The Crucial Role of Prompt UTI Treatment
Urinary tract infections (UTIs) are a significant risk factor for bladder wall calcification. Prompt and effective treatment of UTIs is critical in preventing chronic inflammation and subsequent calcification.
Recognizing UTI Symptoms Early
Being aware of UTI symptoms is crucial for seeking timely medical attention. Common symptoms include:
- Frequent urination
- Urgency
- Pain or burning sensation during urination
- Cloudy or bloody urine
- Pelvic pain or pressure
If you experience any of these symptoms, consult a healthcare professional immediately.
Adhering to Prescribed Treatment Plans
Complete the entire course of antibiotics prescribed by your doctor, even if you start feeling better before the medication is finished. This helps ensure that the infection is completely eradicated and reduces the risk of recurrence.
Skipping doses or stopping treatment prematurely can lead to antibiotic resistance and chronic infection, increasing the likelihood of complications like bladder wall calcification.
Preventing Recurrent UTIs: A Proactive Approach
For individuals prone to recurrent UTIs, proactive measures can help minimize the risk. These include:
- Drinking cranberry juice or taking cranberry supplements (consult with your doctor first).
- Wiping from front to back after using the toilet.
- Urinating after sexual activity.
- Avoiding irritating feminine hygiene products.
In conclusion, while complete prevention of bladder wall calcification may not always be feasible, adopting these lifestyle and dietary recommendations, coupled with prompt and effective treatment of UTIs, can significantly reduce your risk and promote optimal bladder health. Proactive management is key to minimizing potential complications and maintaining a good quality of life.
FAQ: Bladder Wall Calcification
Understanding bladder wall calcification can be complex. Here are some frequently asked questions to clarify the key points.
What exactly is bladder wall calcification?
Bladder wall calcification refers to the buildup of calcium deposits within the tissues of the bladder wall. This can occur due to various underlying conditions. The detection of calcification in bladder wall typically involves imaging techniques.
What are the common causes of calcification in the bladder wall?
Several factors can contribute, including chronic infections, schistosomiasis (a parasitic disease), bladder tumors, and even certain metabolic disorders. The underlying cause needs to be identified for effective management of the calcification in bladder wall.
How is bladder wall calcification usually diagnosed?
Diagnosis often involves a combination of imaging tests, such as X-rays, CT scans, or ultrasounds. These techniques can visualize the calcium deposits within the bladder wall. Your doctor will analyze the images along with your medical history.
Are there always noticeable symptoms if I have calcification in my bladder wall?
Not always. In some cases, bladder wall calcification might be asymptomatic and only discovered during imaging for another reason. However, depending on the underlying cause and the extent of calcification, symptoms like frequent urination, pain, or blood in the urine may occur.
So, there you have it! Hopefully, this helped shed some light on calcification in bladder wall. If you’re still curious or have any lingering questions, definitely chat with your doctor – they’re the real experts. Until next time!