Calcitonin, a hormone produced by the parathyroid gland, plays a significant part in maintaining calcium homeostasis. The question of what is the role of calcitonin in calcium homeostasis? frequently arises when considering skeletal health. Bone resorption, a process regulated in part by calcitonin, impacts the concentration of calcium circulating within the bloodstream. Effective management of calcium levels, supported by knowledge gleaned from medical research institutions like the Mayo Clinic, is essential for overall well-being.
Calcium, often associated with strong bones and teeth, plays a far more pervasive role in human physiology. It is an essential mineral, a critical electrolyte, and a key signaling molecule governing a vast array of bodily functions.
From nerve impulse transmission and muscle contraction to blood clotting and enzyme activity, calcium’s influence is undeniable. However, the body’s ability to utilize calcium effectively hinges on maintaining a remarkably precise balance – a state known as calcium homeostasis.
The Significance of Calcium Homeostasis
Calcium homeostasis refers to the body’s sophisticated mechanisms for maintaining a stable concentration of calcium in the blood and extracellular fluid. This tightly regulated process is not merely about ensuring sufficient calcium levels; it’s equally about preventing excessive accumulation.
Too little calcium (hypocalcemia) can lead to muscle spasms, nerve dysfunction, and even cardiac arrhythmias. Conversely, too much calcium (hypercalcemia) can result in kidney stones, bone weakness, and neurological problems.
The body, therefore, employs a complex interplay of hormones, organs, and feedback loops to keep calcium levels within a narrow, optimal range. This is achieved through:
- Absorption from the diet
- Storage in the bones
- Excretion via the kidneys.
When any of these processes falter, the delicate balance is disrupted, potentially leading to significant health consequences.
Calcitonin: The Underappreciated Regulator
While parathyroid hormone (PTH) and vitamin D are widely recognized for their roles in calcium regulation, calcitonin often remains a less celebrated player. Calcitonin, a peptide hormone produced by the thyroid gland, acts primarily to lower blood calcium levels when they become too high.
While its role is less pronounced than that of PTH, calcitonin contributes significantly to maintaining calcium equilibrium, particularly during periods of rapid bone growth or calcium excess. It’s a crucial component of the body’s multifaceted strategy for safeguarding calcium homeostasis.
This article will delve into the multifaceted role of calcitonin in maintaining calcium homeostasis, exploring its mechanisms of action, its interactions with other key regulators, and its therapeutic applications.
While parathyroid hormone (PTH) and Vitamin D often steal the spotlight in discussions about calcium regulation, the equally important hormone calcitonin quietly exerts its influence. Understanding calcitonin, its origins, and its mechanisms is key to appreciating the body’s sophisticated system for maintaining calcium balance.
What is Calcitonin? Unveiling the Hormone
Calcitonin, in its simplest definition, is a peptide hormone. This means it’s a relatively small protein-based molecule. Its primary function is to lower blood calcium levels when they rise too high. This crucial hormone is synthesized and secreted by a specific population of cells residing within the thyroid gland.
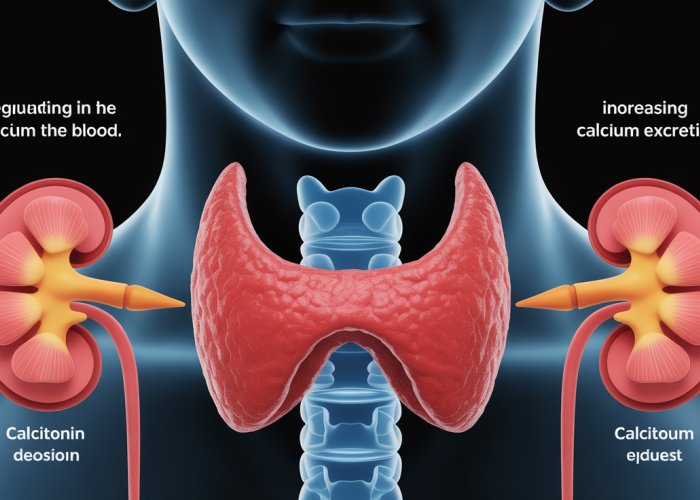
The Thyroid Gland’s Role
The thyroid gland, located in the neck, is primarily known for producing hormones that regulate metabolism. However, it also houses the parafollicular cells, or C-cells, which are the dedicated producers of calcitonin. These cells are interspersed between the follicles of the thyroid, hence their name.
When C-cells detect elevated levels of calcium in the bloodstream, they respond by releasing calcitonin into circulation. This release initiates a cascade of effects designed to bring calcium levels back within the normal range.
Molecular Structure and Function
Calcitonin’s molecular structure is directly related to its biological activity. It consists of a chain of amino acids arranged in a specific sequence. This sequence dictates how the hormone interacts with its target cells, primarily osteoclasts in bone.
The calcitonin molecule binds to specific receptors on osteoclasts, effectively inhibiting their activity. Understanding this molecular interaction is crucial for comprehending calcitonin’s precise role in bone remodeling and calcium regulation. The specific amino acid sequence allows for a lock-and-key fit with the calcitonin receptor, ensuring targeted action.
The intricacies of calcitonin’s molecular structure give us insights to the mechanism of action of how calcitonin contributes to bone health and overall calcium regulation in the body. With a grasp on calcitonin’s origins and basic function, we can now explore the specific ways in which this hormone exerts its influence on calcium levels.
Calcitonin’s Primary Action: Lowering Blood Calcium Levels Explained
At its core, calcitonin is a hypocalcemic hormone.
This means its primary function is to decrease blood calcium levels when they become elevated beyond the normal physiological range.
This action is crucial for preventing hypercalcemia, a condition that can lead to various health problems.
Targeting Osteoclasts: The Key Mechanism
The primary mechanism through which calcitonin lowers blood calcium involves targeting osteoclasts.
These are specialized cells responsible for bone resorption.
Bone resorption is the process where bone tissue is broken down. This releases calcium and other minerals into the bloodstream.
Calcitonin directly inhibits osteoclast activity.
This inhibition is achieved through the binding of calcitonin to specific receptors located on the surface of osteoclasts.
Inhibiting Bone Resorption and Calcium Release
When calcitonin binds to its receptors on osteoclasts, it triggers a cascade of intracellular signaling events.
These events effectively reduce the activity of osteoclasts.
As a result, the rate of bone resorption decreases.
This leads to a reduction in the release of calcium from bone into the bloodstream.
The overall effect is a lowering of blood calcium levels.
This mechanism is especially important during periods of rapid bone turnover. Such as growth spurts or pregnancy. Or in conditions where excessive bone resorption occurs.
Calcitonin’s Influence on Osteoblasts
While calcitonin’s primary target is osteoclasts, it’s important to briefly touch upon its effects, or lack thereof, on osteoblasts.
Osteoblasts are cells responsible for bone formation.
While some studies suggest that calcitonin might have a stimulatory effect on osteoblast activity, this effect is not as pronounced or consistently observed as its inhibitory effect on osteoclasts.
The prevailing understanding is that calcitonin’s dominant role is in reducing bone resorption rather than actively promoting bone formation. The hormone reduces bone remodeling and encourages bone mineral density.
When calcitonin steps in to gently lower calcium levels, it’s not working in isolation. The body’s calcium regulation system is a complex interplay of hormones and organs, each with its own role to play. To fully appreciate calcitonin’s contribution, it’s essential to understand how it interacts with its partners and rivals in maintaining this delicate balance.
Calcitonin’s Partners and Rivals: A Symphony of Hormones
Maintaining calcium homeostasis is not a solo performance but rather a carefully orchestrated symphony. Calcitonin plays a crucial role, but it interacts closely with other hormones and organs. These include parathyroid hormone (PTH), vitamin D, and the kidneys. These interactions are essential for fine-tuning calcium levels and ensuring overall health.
The Dance with Parathyroid Hormone (PTH)
Perhaps calcitonin’s most significant interaction is with parathyroid hormone (PTH). These two hormones function as opposing forces, creating a feedback loop that tightly regulates blood calcium. Understanding this dynamic is crucial for grasping the intricacies of calcium homeostasis.
PTH: The Calcium Elevator
While calcitonin lowers blood calcium, PTH raises it. When calcium levels dip too low, the parathyroid glands release PTH.
PTH acts on several target tissues to increase blood calcium. It stimulates osteoclasts to break down bone, releasing calcium into the bloodstream. It also enhances calcium reabsorption in the kidneys. This prevents calcium from being lost in the urine. Furthermore, PTH indirectly promotes calcium absorption in the intestines by stimulating the production of vitamin D.
An Antagonistic Relationship
The relationship between calcitonin and PTH is antagonistic. When blood calcium is high, calcitonin is released to lower it. Conversely, when blood calcium is low, PTH is released to raise it.
This opposing action creates a negative feedback loop. This ensures that calcium levels remain within a narrow, healthy range.
This balance is essential for proper nerve and muscle function, bone health, and various other physiological processes.
Vitamin D: The Absorption Enhancer
Vitamin D, though not a hormone in the strictest sense, plays a vital role in calcium homeostasis. It primarily influences calcium absorption in the gut. This ensures that the body has an adequate supply of calcium to begin with.
Facilitating Calcium Uptake
Vitamin D promotes the absorption of calcium from the small intestine into the bloodstream. Without sufficient vitamin D, the body can only absorb a fraction of the calcium consumed through diet.
This is why vitamin D deficiency can lead to calcium deficiency, even if dietary intake is adequate.
The active form of vitamin D, calcitriol, binds to receptors in the intestinal cells. This increases the expression of proteins responsible for calcium transport.
A Complex Interplay
The interplay between vitamin D and calcitonin is indirect but significant. Vitamin D ensures that there’s enough calcium available for the body to use. Calcitonin then helps manage the excess when levels rise too high. PTH also plays a role by stimulating vitamin D production in the kidneys when calcium levels are low.
This coordinated action ensures a constant and adequate supply of calcium for all bodily functions.
The Kidneys’ Contribution: Fine-Tuning Excretion
The kidneys are another key player in calcium homeostasis. They act as a filter, regulating how much calcium is excreted in the urine.
Calcium Reabsorption and Excretion
The kidneys can reabsorb calcium back into the bloodstream. They can also excrete excess calcium in the urine.
This process is tightly regulated by hormones, including PTH. PTH increases calcium reabsorption in the kidneys, preventing calcium loss when blood levels are low. Calcitonin, on the other hand, may have a minor effect on reducing calcium reabsorption in the kidneys, but this effect is less pronounced than its impact on osteoclasts.
A Multifaceted Approach
The kidneys’ ability to fine-tune calcium excretion ensures that the body doesn’t lose too much or retain too much of this vital mineral. This function complements the actions of calcitonin, PTH, and vitamin D in maintaining overall calcium balance. By understanding these intricate interactions, we gain a deeper appreciation for the complexity and elegance of the body’s calcium regulation system.
The relationship between calcitonin and PTH forms a finely tuned system. When blood calcium rises, calcitonin is released to bring it down; when it dips, PTH steps in to elevate it. But what happens when this delicate balance is disrupted, leading to conditions of either excess or deficiency in calcium? How does calcitonin function in these scenarios?
Calcitonin’s Role in Calcium Imbalances: Hypercalcemia and Hypocalcemia
Calcium homeostasis, while usually tightly regulated, can sometimes falter. This leads to imbalances like hypercalcemia (excessively high calcium levels) and hypocalcemia (abnormally low calcium levels). Calcitonin’s role is most evident, and therapeutically useful, in managing hypercalcemia. Its function in hypocalcemia is less prominent and still under investigation.
Calcitonin’s Action in Hypercalcemia
Hypercalcemia can arise from various conditions. These include hyperparathyroidism (overactive parathyroid glands), certain cancers, excessive vitamin D intake, and some medications. Regardless of the cause, the primary concern is the dangerously elevated blood calcium.
Here, calcitonin acts as a crucial counter-regulatory hormone. It works swiftly to lower calcium levels back to a safe range.
Mechanisms of Action in Hypercalcemia
Calcitonin’s efficacy in treating hypercalcemia stems from its ability to:
-
Inhibit Osteoclast Activity: This is the primary mechanism. By directly suppressing osteoclast function, calcitonin reduces bone resorption. Consequently, the release of calcium from bone into the bloodstream is significantly reduced.
-
Promote Calcium Excretion by the Kidneys: Calcitonin also modestly enhances calcium excretion by the kidneys. This helps to remove excess calcium from the circulation.
Importantly, while calcitonin is effective in rapidly lowering calcium, its effects are often short-lived. The body can develop resistance to its effects over time, limiting its long-term utility in chronic hypercalcemia management.
Calcitonin and Hypocalcemia: A Less Defined Role
In contrast to its clear role in hypercalcemia, calcitonin’s involvement in hypocalcemia is less direct and not therapeutically significant. Hypocalcemia typically arises from conditions such as:
- Parathyroid hormone deficiency (hypoparathyroidism).
- Vitamin D deficiency.
- Kidney disease.
Because the primary issue in hypocalcemia is insufficient calcium, administering calcitonin, which lowers calcium, would be counterproductive. PTH and vitamin D play much more central roles in restoring calcium balance in these cases.
While calcitonin secretion is suppressed in response to hypocalcemia, this is a passive effect. The body prioritizes PTH release to raise calcium levels. Calcitonin’s absence simply prevents further calcium reduction.
Calcitonin Deficiency: What Happens When It’s Missing?
Unlike deficiencies in PTH or vitamin D, which lead to significant calcium imbalances, the consequences of calcitonin deficiency are generally subtle and often unnoticeable. This is because other regulatory mechanisms can compensate for the lack of calcitonin.
The thyroid gland’s primary function is to produce thyroid hormones, not calcitonin. Therefore, calcitonin deficiency is usually only a consideration after a total thyroidectomy.
However, even in these cases, the body adapts. Blood calcium levels are usually maintained within a normal range by PTH and vitamin D. Some studies suggest that long-term calcitonin deficiency might contribute to slightly increased bone turnover. However, this effect is usually minor and doesn’t typically lead to clinically significant bone disorders.
In essence, while calcitonin is a valuable tool in managing hypercalcemia, its absence is usually well-tolerated. This underscores the hierarchical nature of calcium regulation. PTH and vitamin D are the dominant players, while calcitonin provides a supportive, albeit important, role.
Hypercalcemia and hypocalcemia highlight the critical importance of maintaining calcium balance. But calcitonin’s influence extends beyond these states. The hormone has found specific and important applications in clinical medicine, leveraging its calcium-lowering and bone-protective properties.
Clinical Applications of Calcitonin: Therapeutic Uses
Calcitonin, beyond its fundamental role in calcium homeostasis, has carved a niche in therapeutic medicine. Its ability to modulate calcium levels and influence bone metabolism has led to its use in specific clinical scenarios. While not a first-line treatment for all conditions, calcitonin offers a valuable tool in managing certain diseases and provides a unique therapeutic avenue.
Calcitonin in Hypercalcemia Management
One of the most established applications of calcitonin lies in the treatment of hypercalcemia, particularly in cases where rapid reduction of blood calcium is crucial.
This includes instances of hypercalcemia of malignancy, where cancer cells release substances that promote bone resorption and calcium release.
Calcitonin, often administered intravenously or subcutaneously, can quickly inhibit osteoclast activity and decrease the influx of calcium into the bloodstream. It’s often used as a temporizing measure, providing a bridge to more definitive treatments that address the underlying cause of hypercalcemia. It’s important to note that while effective for rapid calcium reduction, the effect of calcitonin may diminish over time due to receptor downregulation.
This phenomenon, known as escape, limits its long-term utility in managing chronic hypercalcemia.
Calcitonin and Osteoporosis: A Bone-Protective Agent
Calcitonin has also been investigated and utilized in the management of osteoporosis, a condition characterized by decreased bone density and increased fracture risk.
While not as potent as other osteoporosis medications like bisphosphonates, calcitonin offers a unique mechanism of action by directly inhibiting osteoclast activity. This inhibition reduces bone resorption and can contribute to increased bone mineral density, particularly in the spine.
Calcitonin is often considered as an alternative treatment option for individuals who cannot tolerate or have contraindications to other osteoporosis medications. It also has the added benefit of providing analgesic effects, potentially reducing bone pain associated with osteoporotic fractures.
Calcitonin’s Historical Role in Paget’s Disease
Historically, calcitonin played a significant role in the treatment of Paget’s disease of bone, a chronic disorder characterized by abnormal bone remodeling. In Paget’s disease, osteoclasts become overactive, leading to disorganized bone growth and pain.
Calcitonin’s ability to inhibit osteoclast activity helped to normalize bone turnover, reduce pain, and improve bone structure. While other treatments, such as bisphosphonates, have largely replaced calcitonin as first-line therapy for Paget’s disease, it may still be considered in specific cases where bisphosphonates are contraindicated or ineffective.
Delivery Methods and Considerations
Calcitonin is available in different forms, including injectable and nasal spray formulations.
The choice of delivery method depends on factors such as patient preference, convenience, and the specific indication. The nasal spray formulation offers a non-invasive alternative to injections, but its bioavailability may be lower.
It’s important to be aware of potential side effects associated with calcitonin use, such as nausea, flushing, and local injection site reactions. In rare cases, hypersensitivity reactions can occur. As with any medication, the benefits and risks of calcitonin therapy should be carefully considered in consultation with a healthcare professional.
Calcitonin: Your Calcium Homeostasis Questions Answered!
Here are some frequently asked questions about calcitonin and its role in maintaining calcium balance.
How does calcitonin lower blood calcium levels?
Calcitonin acts primarily by inhibiting the activity of osteoclasts, the cells responsible for breaking down bone and releasing calcium into the bloodstream. This effectively reduces calcium release from bone, lowering blood calcium levels. What is the role of calcitonin in calcium homeostasis? In essence, it serves as a counterbalance to parathyroid hormone (PTH), which raises blood calcium.
When is calcitonin released into the bloodstream?
Calcitonin is secreted by the parafollicular cells (C-cells) of the thyroid gland in response to high levels of calcium in the blood (hypercalcemia). The release is directly proportional to the calcium concentration.
What are the main differences between calcitonin and parathyroid hormone (PTH)?
While both calcitonin and parathyroid hormone are vital in calcium homeostasis, they have opposing effects. Calcitonin lowers blood calcium levels, while PTH increases them. What is the role of calcitonin in calcium homeostasis? It counteracts PTH’s effects, maintaining a balance. PTH also affects phosphate levels, which calcitonin doesn’t significantly influence.
Is calcitonin deficiency a common problem?
Calcitonin deficiency is relatively rare and often doesn’t cause any noticeable symptoms. This is because other calcium-regulating mechanisms, like PTH and vitamin D, can compensate. Its impact is less pronounced compared to PTH deficiencies because what is the role of calcitonin in calcium homeostasis? It’s a backup system more than a primary regulator.
So, there you have it! Hopefully, you now have a better understanding of what is the role of calcitonin in calcium homeostasis? It’s pretty fascinating stuff, right? Keep this knowledge handy, and you’ll be the calcium homeostasis expert among your friends!