Understanding the structure of heart is fundamental to grasping cardiovascular physiology. The cardiac chambers, including the atria and ventricles, are integral components responsible for blood flow management. Anatomical models provide visual representations aiding in comprehension of the heart’s complex arrangement. Moreover, cardiology, as a medical field, deeply relies on precise knowledge of the structure of heart for diagnostics and treatment planning. So, let’s dive deep into the architecture of this vital organ using our complete visual guide.
The heart, a remarkable organ, stands as the tireless engine of life.
It orchestrates the circulatory system, a vast network responsible for delivering oxygen, nutrients, hormones, and immune cells.
Equally important, it collects waste products from every corner of our being.
This article serves as a comprehensive guide, offering a detailed and visually engaging exploration of the heart’s complex architecture.
It aims to provide clarity and deeper appreciation for this vital organ.
The Heart: Central Hub of Circulation
At its core, the heart functions as a sophisticated pump.
It tirelessly propels blood throughout the body’s intricate network of vessels.
This continuous circulation is fundamental to sustaining life.
Each heartbeat is a precisely timed event, ensuring that every cell receives the essential elements it needs to thrive.
Why Understanding the Heart Matters
Comprehending the heart’s structure is not merely an academic exercise.
It offers invaluable insights into overall health and well-being.
A solid understanding can empower individuals to make informed decisions regarding lifestyle choices, preventative measures, and early detection of potential cardiac issues.
By knowing how the heart is built, we can better appreciate its function.
We can also recognize potential warning signs of cardiovascular problems, thus allowing for more proactive healthcare management.
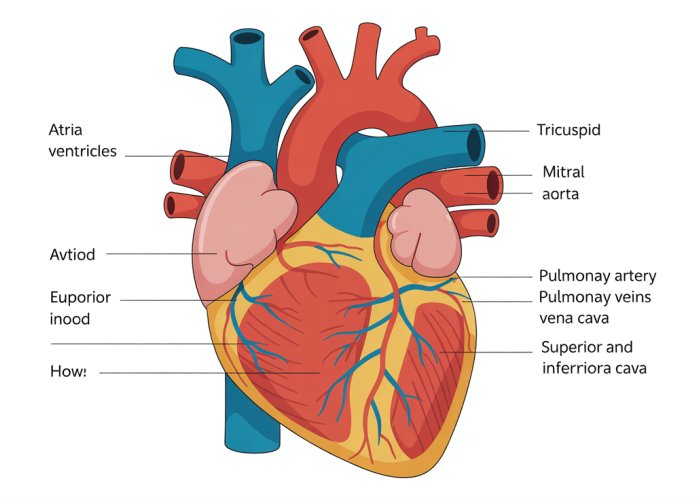
The continuous cycle of blood flow relies on a meticulously organized structure, and the heart’s chambers are at the very heart of this process. These chambers, four in total, work in perfect synchrony to ensure that blood is efficiently circulated throughout the body. Understanding the individual roles of these chambers – the atria and ventricles – is fundamental to grasping the heart’s overall function.
The Heart’s Chambers: A Four-Part Division
The heart is divided into four distinct chambers: two upper chambers called the atria, and two lower chambers called the ventricles. Each chamber plays a vital role in receiving and pumping blood, ensuring the continuous circulation necessary for life. The atria act as receiving stations, while the ventricles serve as the powerful pumps that propel blood either to the lungs or to the rest of the body.
The Atria (Right and Left): Receiving Chambers
The atria, the heart’s two upper chambers, are primarily responsible for receiving blood returning to the heart. The right atrium receives deoxygenated blood from the body, while the left atrium receives oxygenated blood from the lungs.
Right Atrium: Receiving Deoxygenated Blood
Positioned on the upper right side of the heart, the right atrium is the entry point for deoxygenated blood returning from the body. Blood enters the right atrium via two major veins: the superior vena cava, which carries blood from the upper body, and the inferior vena cava, which carries blood from the lower body.
Once in the right atrium, the blood is temporarily held before being passed through the tricuspid valve into the right ventricle.
Left Atrium: Receiving Oxygenated Blood
The left atrium, situated on the upper left side of the heart, receives oxygenated blood from the lungs. This oxygen-rich blood flows into the left atrium through the pulmonary veins. These veins are unique in that they are the only veins in the body that carry oxygenated blood.
From the left atrium, the oxygenated blood flows through the mitral valve into the left ventricle.
The Atrial Septum: Dividing the Receiving Chambers
Separating the right and left atria is a wall of tissue called the atrial septum. This septum prevents the mixing of deoxygenated and oxygenated blood, ensuring that the blood remains separated based on its oxygen content. This separation is critical for efficient oxygen delivery to the body.
The Ventricles (Right and Left): Pumping Powerhouses
The ventricles, located beneath the atria, are the heart’s primary pumping chambers. Their muscular walls contract to forcefully eject blood either to the lungs for oxygenation (right ventricle) or to the rest of the body (left ventricle).
Right Ventricle: Pumping Blood to the Lungs
The right ventricle receives deoxygenated blood from the right atrium. When the right ventricle contracts, it pumps this blood through the pulmonary valve into the pulmonary artery, which carries the blood to the lungs.
In the lungs, the blood releases carbon dioxide and picks up oxygen, becoming oxygenated.
Left Ventricle: Pumping Blood to the Body
The left ventricle, the largest and most muscular chamber of the heart, receives oxygenated blood from the left atrium. Its powerful contractions pump this blood through the aortic valve into the aorta, the body’s largest artery.
The aorta then branches into a network of smaller arteries, delivering oxygenated blood to all parts of the body.
The Ventricular Septum: Dividing the Pumping Chambers
Similar to the atrial septum, the ventricular septum is a wall of tissue that separates the right and left ventricles. This septum is essential for preventing the mixing of oxygenated and deoxygenated blood within the heart.
Myocardial Thickness: A Reflection of Pumping Power
The myocardium, the muscular wall of the heart, varies in thickness between the two ventricles. The left ventricle has a significantly thicker myocardial wall than the right ventricle. This difference in thickness reflects the different workloads of the two chambers.
The left ventricle must generate enough force to pump blood throughout the entire body, while the right ventricle only needs to pump blood to the nearby lungs. The increased thickness of the left ventricle’s myocardium allows it to generate the higher pressure needed for systemic circulation.
The Heart Valves: Guardians of Blood Flow
With the chambers of the heart acting as the engine, and the atria and ventricles diligently pumping, there needs to be a system in place to ensure the blood flows in the correct direction. This is where the heart valves come into play. These ingenious structures are the guardians of unidirectional blood flow, ensuring that blood moves efficiently and effectively through the heart. Let’s explore these vital components and understand how they prevent backflow, maintaining the continuous circulation essential for life.
Overview of Heart Valves: Ensuring One-Way Flow
The heart relies on a quartet of meticulously designed valves. Their sole purpose is to enforce a one-way passage of blood, preventing any retrograde movement. These valves act as gates, opening to allow blood to flow forward and closing tightly to prevent it from flowing backward.
This unidirectional flow is absolutely critical. Without it, the heart’s pumping action would become chaotic and inefficient, jeopardizing the entire circulatory system.
The consequences of valve malfunction can range from mild fatigue to severe heart failure, highlighting the importance of these unsung heroes of the cardiovascular system.
The Tricuspid Valve: Right Atrium to Right Ventricle
Located between the right atrium and the right ventricle, the tricuspid valve gets its name from its three leaflets, or cusps. This valve acts as a gatekeeper, opening to allow deoxygenated blood to flow from the right atrium into the right ventricle.
During ventricular contraction, the tricuspid valve snaps shut. This prevents the backflow of blood into the right atrium, ensuring that blood is propelled forward into the pulmonary artery. Proper function of the tricuspid valve is essential for maintaining efficient circulation to the lungs.
The Mitral Valve (Bicuspid Valve): Left Atrium to Left Ventricle
On the left side of the heart, the mitral valve – also known as the bicuspid valve – controls blood flow between the left atrium and the left ventricle. Unlike the tricuspid valve, the mitral valve has two leaflets.
This valve opens to allow oxygenated blood from the lungs to flow into the left ventricle. Then, during ventricular contraction, the mitral valve closes tightly, preventing blood from flowing back into the left atrium. The mitral valve’s proper function is crucial for ensuring that oxygen-rich blood is efficiently pumped out to the body.
The Pulmonary Valve: Right Ventricle to Pulmonary Artery
The pulmonary valve sits between the right ventricle and the pulmonary artery. This valve’s task is to regulate blood flow from the right ventricle into the pulmonary artery, the vessel that carries deoxygenated blood to the lungs for oxygenation.
The pulmonary valve opens when the right ventricle contracts, allowing blood to flow into the pulmonary artery. Once the ventricle relaxes, the pulmonary valve closes, preventing blood from flowing back into the right ventricle. This ensures that blood moves in the correct direction toward the lungs.
The Aortic Valve: Left Ventricle to Aorta
The aortic valve is positioned between the left ventricle and the aorta, the body’s largest artery. It’s a critical valve. Its function is to control the flow of oxygenated blood from the left ventricle into the aorta, which distributes it to the rest of the body.
Role of Chordae Tendineae and Papillary Muscles
When the left ventricle contracts, the aortic valve opens, allowing blood to surge into the aorta. Then, as the ventricle relaxes, the aortic valve closes, preventing backflow into the left ventricle.
Uniquely, the mitral and tricuspid valves are connected to chordae tendineae, which are strong, fibrous cords that attach to papillary muscles within the ventricles. These structures are essential for valve function. The papillary muscles contract along with the ventricle.
The chordae tendineae prevent the valve leaflets from prolapsing, or bulging backward, into the atria during ventricular contraction. This support system ensures a tight seal, preventing leakage and maintaining unidirectional blood flow.
The tricuspid, mitral, pulmonary, and aortic valves meticulously control the flow of blood, preventing backflow and ensuring that each chamber efficiently contributes to the circulatory process. But what encases and supports these chambers and valves, providing the structural integrity necessary for the heart’s relentless work? The answer lies in the heart wall, a sophisticated three-layered structure that not only protects the heart but also plays a crucial role in its function.
The Heart Wall: A Three-Layered Structure
The heart, that tireless engine of life, isn’t just a hollow pump. Its wall is composed of three distinct layers, each with a specialized role: the pericardium (outer layer), the myocardium (middle layer), and the endocardium (inner layer). These layers work in concert to provide protection, structural support, and the essential contractile force needed to circulate blood throughout the body.
The Pericardium: Protective Outer Layer
The pericardium is a double-layered sac that surrounds the heart, providing protection and reducing friction. It’s like a bodyguard for the heart, shielding it from external forces and ensuring it can beat smoothly within the chest cavity.
Fibrous Pericardium
The outer layer of the pericardium is the fibrous pericardium, a tough, inelastic sac made of dense connective tissue. This layer anchors the heart within the mediastinum, preventing it from overexpanding and limiting its movement.
Serous Pericardium
The inner layer of the pericardium is the serous pericardium, which itself has two layers:
-
Parietal Layer: This layer is fused to the fibrous pericardium.
-
Visceral Layer (Epicardium): This layer is directly attached to the heart and is considered part of the heart wall itself.
Between the parietal and visceral layers is the pericardial cavity, a space filled with a small amount of serous fluid. This fluid acts as a lubricant, reducing friction as the heart beats.
The Myocardium: Muscular Middle Layer
The myocardium is the thickest layer of the heart wall and is composed of cardiac muscle tissue. This is the layer responsible for the heart’s powerful contractions.
The arrangement of muscle fibers within the myocardium is complex and allows the heart to squeeze blood out of the chambers efficiently. The thickness of the myocardium varies depending on the chamber; the ventricles, which pump blood to the lungs and body, have thicker walls than the atria.
Cardiac Muscle Tissue
Cardiac muscle tissue is unique. Its cells are striated, like skeletal muscle, but are involuntary, meaning we don’t consciously control their contractions.
Cardiac muscle cells are connected by intercalated discs, which contain gap junctions that allow electrical impulses to spread rapidly from cell to cell. This allows the heart to contract in a coordinated manner.
Cardiac muscle also has a long refractory period, which prevents tetanus (sustained contraction) and ensures that the heart has time to relax and refill between beats.
The Endocardium: Inner Lining
The endocardium is the innermost layer of the heart wall. It’s a thin, smooth layer of endothelium that lines the heart chambers and covers the valves.
Its primary function is to minimize friction as blood flows through the heart, ensuring smooth and efficient circulation. The endocardium is continuous with the endothelium of the blood vessels that enter and leave the heart. This continuity helps to prevent blood clots from forming within the heart.
The health of the endocardium is crucial for preventing conditions like endocarditis, an infection of the inner lining of the heart.
Blood Vessels of the Heart: Fueling and Supplying Life
The heart, for all its intricate chambers, valves, and layers, is fundamentally reliant on a network of blood vessels to sustain its ceaseless activity and, indeed, to sustain life itself. These vessels, both arteries and veins, are the highways and byways of the circulatory system, ensuring that the heart muscle receives the oxygen and nutrients it needs, while also facilitating the critical exchange of gases and waste products. Without this intricate vascular network, the heart would quickly cease to function, with dire consequences for the entire organism.
Coronary Arteries: Nourishing the Heart Muscle
The Heart’s Lifeline
The coronary arteries are of paramount importance, serving as the lifeline that delivers oxygenated blood directly to the myocardium, the heart muscle itself. Arising from the aorta near its origin, these arteries, the left and right coronary arteries, branch out to encircle the heart, ensuring that every part of the myocardium receives a constant supply of oxygen and nutrients.
These arteries are working constantly, delivering the crucial blood that the heart needs to power all of its functions.
The Peril of Coronary Artery Disease
Given their vital role, any compromise to the coronary arteries can have devastating consequences. Coronary artery disease (CAD), typically caused by the buildup of plaque within the arterial walls (atherosclerosis), can restrict blood flow, leading to angina (chest pain) or, in severe cases, myocardial infarction (heart attack).
In these cases, the heart muscle is unable to properly function due to the lack of sufficient blood to power it. CAD is a leading cause of death worldwide, highlighting the critical importance of maintaining healthy coronary arteries through lifestyle choices and medical interventions.
Aorta and Pulmonary Artery: Major Arterial Outlets
The Aorta: The Body’s Main Artery
The aorta, the largest artery in the body, emerges directly from the left ventricle, carrying oxygenated blood under high pressure to the systemic circulation. This blood is destined for every tissue and organ in the body. Its sheer size and strategic location makes it a critical link in the circulatory system.
The aorta’s robust structure is essential to withstand the forceful ejection of blood with each heartbeat, ensuring a constant and reliable supply of oxygen and nutrients to the entire body.
The Pulmonary Artery: To the Lungs for Oxygenation
In contrast to the aorta, the pulmonary artery carries deoxygenated blood from the right ventricle to the lungs. This is the start of the pulmonary circuit, where blood releases carbon dioxide and picks up a fresh supply of oxygen via the alveoli.
The pulmonary artery is unique because it is the only artery in the body that carries deoxygenated blood. Its critical role in the process of oxygenating the blood makes it vital to the functioning of the body.
Vena Cava and Pulmonary Veins: Returning Blood to the Heart
Vena Cava: Returning Blood from the Body
The superior and inferior vena cava are large veins that return deoxygenated blood from the body back to the right atrium of the heart. The superior vena cava drains blood from the upper body, while the inferior vena cava drains blood from the lower body.
These veins ensure that deoxygenated blood is efficiently returned to the heart, where it can then be pumped to the lungs for re-oxygenation.
Pulmonary Veins: Returning Oxygenated Blood
Finally, the pulmonary veins carry oxygenated blood from the lungs back to the left atrium of the heart. There are typically four pulmonary veins, two from each lung.
These veins are unique as they are the only veins in the body that carry oxygenated blood, completing the circuit and enabling the heart to pump freshly oxygenated blood to the rest of the body via the aorta. Without these veins, the heart would be unable to pump the oxygenated blood that is necessary to sustain life.
Given the intricate network of vessels ensuring the heart’s nourishment, it’s easy to overlook the equally vital system responsible for initiating and coordinating its rhythmic contractions. This system, operating silently and continuously, is the heart’s electrical conduction network, a marvel of biological engineering.
The Heart’s Electrical System: The Conduction Network
The heart is not simply a mechanical pump; it is an electromechanical marvel. Its ability to contract rhythmically and efficiently relies on an intrinsic electrical conduction system that dictates the timing and sequence of each heartbeat. This sophisticated network, comprised of specialized cells, ensures that the atria and ventricles contract in a coordinated manner, maximizing cardiac output and maintaining healthy circulation. The key components of this system are the sinoatrial (SA) node, atrioventricular (AV) node, Bundle of His, and Purkinje fibers.
The Sinoatrial (SA) Node: The Natural Pacemaker
The sinoatrial (SA) node, often referred to as the heart’s natural pacemaker, is a small cluster of specialized cells located in the wall of the right atrium. Its primary function is to generate electrical impulses spontaneously and rhythmically. These impulses initiate each heartbeat, setting the pace for the entire cardiac cycle.
Think of the SA node as the conductor of an orchestra. It sets the tempo, ensuring all other instruments play in harmony.
The SA node’s intrinsic firing rate is approximately 60 to 100 beats per minute, which is why a normal resting heart rate falls within this range. This rate can be influenced by various factors, including the autonomic nervous system, hormones, and medications, allowing the heart to adapt to changing physiological demands.
The Atrioventricular (AV) Node: Delaying and Relaying Impulses
The electrical impulse generated by the SA node travels rapidly through the atria, causing them to contract. This electrical signal then reaches the atrioventricular (AV) node, another cluster of specialized cells located in the septum between the atria and ventricles.
The AV node serves a crucial role: to delay the electrical signal slightly before relaying it to the ventricles. This delay, typically lasting about 0.1 seconds, allows the atria to contract completely and empty their contents into the ventricles before ventricular contraction begins.
Without this delay, the atria and ventricles would contract simultaneously. This would lead to inefficient blood flow and reduced cardiac output.
The AV node also acts as a gatekeeper, preventing excessively rapid atrial impulses from reaching the ventricles. In cases of atrial fibrillation or atrial flutter, where the atria beat very rapidly, the AV node can block some of these impulses, protecting the ventricles from dangerously high rates.
Bundle of His and Purkinje Fibers: Conducting Impulses to the Ventricles
After the AV node delays the electrical signal, it is rapidly transmitted to the ventricles via the Bundle of His and Purkinje fibers.
The Bundle of His is a specialized bundle of conductive fibers that originates in the AV node and travels down the interventricular septum, dividing into the left and right bundle branches. These branches then further divide into a network of fine fibers called Purkinje fibers, which spread throughout the ventricular myocardium.
This network of fibers ensures that the electrical impulse is rapidly and uniformly distributed throughout the ventricles, triggering a coordinated and powerful contraction.
The coordinated ventricular contraction is essential for effectively ejecting blood into the pulmonary artery and aorta, driving systemic circulation.
The Cardiac Cycle and the Electrical System
The cardiac cycle is the sequence of events that occur during one complete heartbeat, including atrial contraction (atrial systole), ventricular contraction (ventricular systole), and relaxation (diastole).
The electrical system directly governs the timing of these events. The SA node initiates atrial systole. The AV node delay ensures complete atrial emptying. The rapid conduction through the Bundle of His and Purkinje fibers initiates ventricular systole.
Any disruption to the heart’s electrical system, such as arrhythmias or heart block, can disrupt the cardiac cycle, leading to inefficient blood flow and potentially life-threatening complications.
Understanding the intricate workings of the heart’s electrical system is crucial for comprehending cardiac function and diagnosing and treating various heart conditions. From the SA node’s rhythmic initiation to the Purkinje fibers’ coordinated distribution, this network is a testament to the heart’s remarkable design and its vital role in sustaining life.
FAQs: Understanding Heart’s Structure
This section answers common questions about the heart’s structure, helping you better understand the visual guide.
What are the main chambers of the heart?
The heart has four main chambers: the left atrium, the right atrium, the left ventricle, and the right ventricle. These chambers work together to pump blood throughout the body. Understanding their role is key to grasping the overall structure of the heart.
How do the valves within the heart function?
Heart valves, including the mitral, tricuspid, aortic, and pulmonary valves, ensure blood flows in one direction. They open and close rhythmically, preventing backflow. These valves are crucial for efficient blood circulation and a vital component of the structure of heart.
What are the major blood vessels connected to the heart?
Key vessels connected to the heart include the aorta, pulmonary artery, pulmonary veins, superior vena cava, and inferior vena cava. Each plays a critical role in transporting blood to and from the heart. They contribute directly to the overall structure of heart’s circulatory system.
What are the layers of the heart wall?
The heart wall consists of three layers: the epicardium (outer layer), the myocardium (middle, muscular layer), and the endocardium (inner layer). Each layer has a specific function and contributes to the heart’s structure and its ability to contract and pump blood effectively.
So, that’s the heart in a nutshell! Hopefully, this complete visual guide has given you a clearer picture of the structure of heart. Keep exploring, keep asking questions, and remember to take care of that amazing pump inside you!