Understanding the nuances of tissue mass pelvis male necessitates exploring associated conditions and diagnostic procedures. The prostate gland, a key entity in male reproductive health, often becomes relevant when discussing tissue masses in the pelvic region. Diagnostic imaging, specifically Magnetic Resonance Imaging (MRI), provides valuable insights into the characteristics and location of such masses. Medical professionals specializing in urology frequently encounter and manage cases involving abnormal tissue growth in the male pelvis. Therefore, the interpretation of findings related to tissue mass pelvis male frequently integrates information from pathology reports and clinical evaluations conducted by experts at institutions like the National Institutes of Health (NIH).
The male pelvic region, a complex network of organs and structures, can sometimes be the site of an abnormal tissue mass. This presence, often discovered during a routine exam or prompted by specific symptoms, can understandably cause concern. Understanding what this tissue mass represents, its potential origins, and the implications for overall health is crucial for informed decision-making and proactive healthcare.
What is a Tissue Mass?
A tissue mass, in its simplest definition, refers to an unusual growth or collection of cells within the body. In the male pelvis, this could manifest in various forms, ranging from benign enlargements to more serious malignant tumors.
The term "mass" is a general descriptor, and its precise nature requires further investigation through medical examination and diagnostic testing. It’s not a diagnosis in itself, but rather a sign that warrants further attention.
Why Understanding Matters
The discovery of a tissue mass in the male pelvis can be unsettling, but knowledge is power. A thorough understanding of the potential causes is paramount.
Knowing the possible origins, which range from benign prostatic hyperplasia (BPH) to cancerous growths, empowers individuals to engage more effectively with their healthcare providers. It facilitates informed discussions about diagnostic and treatment options.
Furthermore, grasping the potential implications for overall health is essential. Some tissue masses may be asymptomatic and pose minimal risk, while others can significantly impact urinary function, sexual health, and even be life-threatening. Early detection and appropriate management are key to minimizing potential adverse outcomes.
Article Objectives
This article aims to provide a comprehensive overview of tissue masses in the male pelvis. Our goal is to equip you with the knowledge necessary to:
- Understand the basic anatomy of the male pelvis and the structures most relevant to tissue mass formation.
- Recognize the potential underlying causes of a tissue mass, both benign and malignant.
- Identify the common symptoms and signs associated with such masses.
- Comprehend the diagnostic process, from initial imaging to definitive biopsy.
- Explore the various treatment options available, emphasizing the importance of a personalized approach.
- Appreciate the roles of different medical specialists in the diagnosis and management of pelvic tissue masses.
By providing this information, we hope to empower you to be an active participant in your healthcare journey, fostering informed decisions and promoting better health outcomes. This article serves as a starting point for understanding, not a substitute for professional medical advice. Always consult with a qualified healthcare provider for any health concerns.
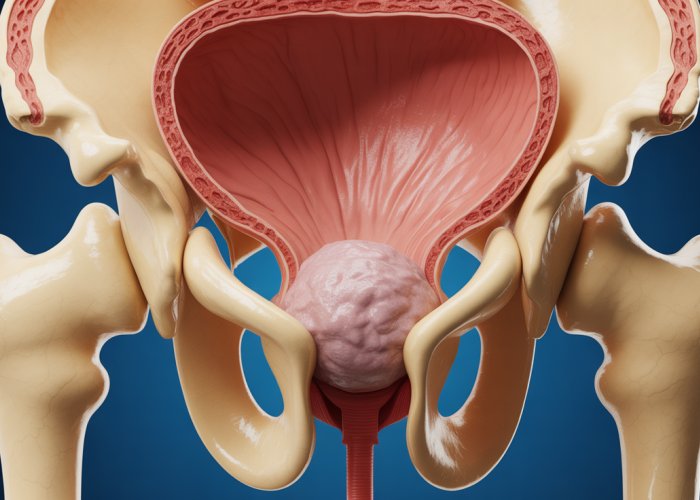
Anatomy 101: Key Structures of the Male Pelvis
Before diving into the potential origins and implications of a tissue mass in the male pelvis, it’s important to establish a firm understanding of the anatomical landscape. This region, a complex interplay of organs and structures, requires careful consideration to appreciate the potential impact of any abnormal growth.
This section provides a concise overview of the key anatomical components, emphasizing those most frequently involved in or affected by the formation of a tissue mass. Grasping these foundational elements will significantly enhance comprehension of subsequent discussions regarding causes, symptoms, and diagnostic approaches.
The Prostate Gland: A Central Player
The prostate gland, often at the forefront of discussions regarding male pelvic health, is a walnut-sized gland located just below the bladder and in front of the rectum. Its primary function is to produce fluid that contributes to semen.
Due to its location and function, the prostate is a common site for tissue mass development, particularly in the form of benign prostatic hyperplasia (BPH) or prostate cancer. Changes in size, shape, or texture of the prostate can be readily detected during a digital rectal exam, making it a crucial area of focus.
Seminal Vesicles: Partners in Reproduction
Positioned behind the bladder and adjacent to the prostate are the seminal vesicles. These glands are responsible for producing a significant portion of the fluid that makes up semen, contributing to sperm motility and viability.
While less frequently the primary site of a tissue mass, the seminal vesicles can be affected by the spread of cancer from nearby organs, such as the prostate. Inflammation or infection can also lead to changes in their structure.
The Bladder: Reservoir and Pathway
The bladder, a muscular sac located in the anterior pelvis, serves as a reservoir for urine before it is expelled from the body. Its connection to the urethra, the tube that carries urine out of the body, makes it susceptible to issues arising from surrounding structures.
A tissue mass in the pelvis can exert pressure on the bladder, leading to urinary symptoms such as frequency, urgency, or difficulty urinating. Primary bladder tumors, though less common, can also manifest as a palpable mass.
The Rectum: Posterior Neighbor
Located behind the prostate and bladder is the rectum, the final section of the large intestine. Due to its proximity, the rectum can be affected by tissue masses originating in adjacent organs.
Conversely, rectal cancer can present as a palpable mass during a rectal exam. The relationship between the rectum and surrounding pelvic structures necessitates careful evaluation when assessing a tissue mass in this region.
Lymph Nodes: Sentinels of the Pelvis
The pelvic lymph nodes are small, bean-shaped structures that play a vital role in the immune system. They filter lymph fluid, trapping bacteria, viruses, and cancer cells.
Enlarged lymph nodes in the pelvis can indicate infection, inflammation, or the spread of cancer from nearby organs. Palpable lymph nodes may be detected during a physical exam or visualized on imaging studies, providing valuable clues about the nature of a tissue mass.
Pelvic Floor Muscles: Support and Function
The pelvic floor muscles form a sling-like structure that supports the pelvic organs, including the bladder, prostate, and rectum. These muscles are essential for urinary and bowel control, as well as sexual function.
While not typically the primary site of a tissue mass, dysfunction or abnormalities in the pelvic floor muscles can contribute to pelvic pain and discomfort. Furthermore, a tissue mass in the pelvis can indirectly affect these muscles, leading to altered function.
Understanding the intricate relationships between these key anatomical structures is paramount when considering the potential causes, symptoms, and treatment strategies for a tissue mass in the male pelvis. This foundational knowledge will serve as a valuable framework for navigating the complexities of this condition.
Seminal vesicles, while not always the primary culprit, can also be affected by masses that impact the male pelvic region. However, to fully grasp the potential complexities surrounding the formation of a tissue mass, we must now turn our attention to the diverse range of underlying causes. Understanding these causes is essential for both preventative measures and informed decision-making during diagnosis and treatment.
Unraveling the Causes: What Can Trigger a Tissue Mass?
The discovery of a tissue mass in the male pelvis can understandably cause concern. It’s crucial to remember that not all masses are cancerous. Many benign conditions can also manifest as a palpable or visible mass. Understanding the spectrum of potential causes is the first step towards informed management.
Tumors: Benign vs. Malignant
The term "tumor" simply refers to an abnormal growth of tissue. Tumors can be broadly classified as either benign or malignant.
- Benign tumors are non-cancerous growths that do not spread to other parts of the body. While they may cause local symptoms due to their size or location, they are generally not life-threatening.
- Malignant tumors, on the other hand, are cancerous and have the potential to invade surrounding tissues and spread to distant sites (metastasis). These tumors require aggressive treatment to control their growth and prevent further spread.
An oncologist, a specialist in cancer treatment, plays a crucial role in diagnosing and managing malignant tumors. Their expertise is essential for determining the appropriate course of action, which may include surgery, radiation therapy, chemotherapy, or a combination of these modalities.
Cancers Affecting the Male Pelvis
Several types of cancer can originate in or spread to the male pelvis, potentially presenting as a tissue mass. Two of the most common include:
- Prostate Cancer: This is one of the most prevalent cancers among men. It originates in the prostate gland and can range from slow-growing, indolent forms to aggressive, rapidly progressing types. Early detection through screening, such as PSA testing and digital rectal exams, is crucial for successful treatment.
- Rectal Cancer: Located in the final section of the large intestine, rectal cancer can also manifest as a mass in the pelvic region. Risk factors include age, family history, and certain lifestyle choices. Colonoscopies are essential for early detection and prevention.
Benign Prostatic Hyperplasia (BPH)
Benign Prostatic Hyperplasia (BPH) is a non-cancerous enlargement of the prostate gland. As men age, the prostate gland often increases in size, which can compress the urethra and lead to urinary symptoms.
While BPH is not cancerous, the enlarged prostate can sometimes be felt as a distinct mass during a physical examination.
The symptoms of BPH can significantly impact quality of life, and treatment options range from lifestyle modifications and medications to minimally invasive procedures or surgery.
Prostatitis: Inflammation as a Potential Cause
Prostatitis refers to inflammation of the prostate gland. It can be caused by bacterial infection or other factors. While not a tumor in the traditional sense, the inflammation and swelling associated with prostatitis can sometimes create a palpable mass or area of tenderness in the prostate region.
Symptoms of prostatitis can vary widely, from mild discomfort to severe pain and urinary problems. Treatment typically involves antibiotics for bacterial infections, along with medications to manage pain and inflammation.
Elaboration on Risk Factors
Several factors can increase the risk of developing the conditions that lead to tissue mass formation in the male pelvis. These risk factors vary depending on the specific underlying cause.
- Age: The risk of many conditions, including BPH and prostate cancer, increases with age.
- Family History: A family history of prostate cancer, rectal cancer, or other pelvic cancers can significantly increase an individual’s risk.
- Lifestyle Factors: Diet, obesity, smoking, and lack of physical activity have been linked to an increased risk of certain pelvic conditions, including some cancers.
- Infections: A history of sexually transmitted infections (STIs) may increase the risk of prostatitis and other inflammatory conditions.
- Race/Ethnicity: African American men have a higher risk of developing prostate cancer compared to other racial groups.
Understanding and managing these risk factors, where possible, is an important aspect of preventative health and early detection. Regular check-ups and screenings, tailored to individual risk profiles, are essential for identifying potential problems early on when treatment is most effective.
Unraveling the causes behind a tissue mass paints a comprehensive picture, yet understanding the potential signals your body might send is equally crucial. It allows for early detection and timely intervention. These signals manifest as various symptoms, which we will explore below.
Decoding the Signals: Recognizing Symptoms and Signs
The presence of a tissue mass in the male pelvis can manifest through a variety of signs and symptoms. However, it’s important to emphasize that the experience can differ significantly from person to person. The intensity, duration, and specific nature of these symptoms often depend on the underlying cause, size, and location of the mass. Being attentive to your body and recognizing potential warning signs is key to seeking timely medical attention.
Common Symptoms Associated with Pelvic Tissue Mass
Several common symptoms may indicate the presence of a tissue mass in the male pelvis. These can range from mild discomfort to severe pain and noticeable changes in bodily functions. Paying attention to these signals and consulting with a healthcare professional is essential for proper evaluation and diagnosis.
Pelvic Pain
Pelvic pain is a frequent complaint among individuals with a tissue mass in the male pelvis. This pain can manifest in various ways:
-
Location: The pain may be localized to a specific area within the pelvis or be more diffuse, spreading across a wider region.
-
Intensity: The intensity of the pain can vary from a dull ache to a sharp, stabbing sensation. It might be constant or intermittent, fluctuating with certain activities or positions.
-
Nature: The nature of the pain can also differ. Some individuals experience a constant, gnawing pain, while others report sharp, shooting pains that come and go.
-
Associated Symptoms: Pelvic pain can sometimes be accompanied by other symptoms, such as tenderness to the touch, muscle spasms, or referred pain in the lower back or legs.
It’s vital to note that pelvic pain can arise from various other conditions. Therefore, a thorough evaluation by a medical professional is crucial to determine the underlying cause and receive appropriate treatment.
Urinary Symptoms
The urinary tract’s proximity to the pelvic organs means that a tissue mass can significantly impact urinary function, which can lead to a cluster of symptoms. These symptoms may include:
-
Increased Urinary Frequency: A frequent urge to urinate, even when the bladder is not full, can indicate pressure or irritation from the mass.
-
Urinary Urgency: A sudden, compelling need to urinate that is difficult to delay.
-
Difficulty Urinating (Hesitancy): Trouble initiating the urine stream or a weak urine flow.
-
Incomplete Bladder Emptying: A sensation that the bladder is not completely emptied after urination.
-
Nocturia: Waking up frequently during the night to urinate.
-
Painful Urination (Dysuria): Discomfort or burning sensation during urination.
These urinary symptoms can greatly impact daily life and should not be ignored.
Symptom Variability
It’s crucial to understand that the symptoms associated with a tissue mass in the male pelvis can vary significantly based on the underlying cause and location of the mass.
For instance, a small, slow-growing benign tumor might not cause any noticeable symptoms initially. In contrast, a rapidly growing malignant tumor could lead to more pronounced and severe symptoms.
The location of the mass also plays a crucial role. A mass near the bladder might primarily cause urinary symptoms.
Similarly, a mass affecting the rectum could result in changes in bowel habits or rectal bleeding. A mass pressing on nerves could lead to pain or numbness in the legs.
Given this variability, it is imperative to seek prompt medical attention for any unexplained or persistent pelvic symptoms. A healthcare professional can conduct a thorough evaluation, determine the underlying cause, and recommend the most appropriate course of action.
Unraveling the causes behind a tissue mass paints a comprehensive picture, yet understanding the potential signals your body might send is equally crucial. It allows for early detection and timely intervention. These signals manifest as various symptoms. Now, let’s shift our focus to the diagnostic procedures that transform suspicion into a confirmed diagnosis, providing a roadmap of the steps involved in identifying and characterizing a tissue mass within the male pelvis.
The Diagnostic Journey: From Suspicion to Confirmation
The path to diagnosing a tissue mass in the male pelvis is often a carefully orchestrated sequence of evaluations, designed to first identify the presence of an abnormality, then characterize its nature, and finally, determine its potential impact on overall health. This journey involves a combination of clinical assessments, advanced imaging techniques, and, ultimately, tissue sampling for definitive analysis.
Initial Assessment and Clinical Evaluation
The diagnostic process typically begins with a thorough clinical evaluation. This often includes:
-
Medical History Review: The doctor will inquire about your medical history, including any pre-existing conditions, medications, and family history of cancer or other relevant diseases.
-
Physical Examination: A physical examination, including a digital rectal exam (DRE), may be performed to assess the prostate and surrounding tissues.
-
Symptom Assessment: A detailed discussion of your symptoms, their duration, and severity.
These initial steps provide valuable clues that guide subsequent diagnostic decisions.
The Power of Medical Imaging
If the initial assessment raises suspicion of a tissue mass, medical imaging becomes essential for visualizing the pelvic region and identifying any abnormalities. Several imaging modalities are commonly employed, each offering unique advantages:
Magnetic Resonance Imaging (MRI)
MRI uses strong magnetic fields and radio waves to create detailed images of the soft tissues within the pelvis. MRI is particularly useful for visualizing the prostate, seminal vesicles, bladder, and rectum. It can help differentiate between different types of tissue and identify even small masses.
Computed Tomography (CT) Scan
CT scans utilize X-rays to create cross-sectional images of the body. CT scans are valuable for assessing the size and location of a tissue mass, as well as for detecting any spread to nearby lymph nodes or other organs.
Ultrasound
Ultrasound uses sound waves to create real-time images of the pelvic organs. Transrectal ultrasound (TRUS) is often used to visualize the prostate. Ultrasound can help guide biopsies and assess the characteristics of a mass.
The choice of imaging modality depends on the specific clinical scenario and the information required. Often, a combination of imaging techniques is used to provide a comprehensive assessment.
The Role of Biopsy in Definitive Diagnosis
While imaging techniques can provide valuable information about the size, location, and characteristics of a tissue mass, a biopsy is typically required to confirm the diagnosis and determine the nature of the mass. A biopsy involves taking a small sample of tissue from the mass for microscopic examination by a pathologist.
Biopsy Techniques
Several biopsy techniques can be used to obtain tissue samples from the male pelvis. These include:
- Needle Biopsy: A thin needle is inserted through the skin or rectum to extract a tissue sample. This can be performed under ultrasound or CT guidance.
- Surgical Biopsy: In some cases, a surgical procedure may be necessary to obtain a larger tissue sample.
Pathological Analysis
The tissue sample obtained during the biopsy is then sent to a pathology lab, where it is carefully examined under a microscope. The pathologist can determine whether the tissue is benign (non-cancerous) or malignant (cancerous) and, if malignant, can identify the specific type of cancer.
The results of the biopsy are crucial for determining the appropriate course of treatment.
Integrating Findings for a Comprehensive Diagnosis
The diagnostic journey culminates in the integration of all available information, including the patient’s medical history, physical examination findings, imaging results, and biopsy results. By carefully analyzing these data, healthcare professionals can arrive at a definitive diagnosis and develop a personalized treatment plan.
The diagnostic process can be a complex and sometimes lengthy endeavor, but it is essential for ensuring accurate diagnosis and effective management of tissue masses in the male pelvis.
The diagnostic journey can feel like navigating a complex maze, but once a tissue mass is identified and characterized, the path forward focuses on treatment. Understanding the landscape of treatment options is crucial for patients and their families. It allows them to participate actively in shared decision-making with their medical team.
Navigating Treatment Options: A Personalized Approach
The management of tissue masses in the male pelvis demands a highly individualized approach. There is no one-size-fits-all solution. The most effective treatment strategy depends significantly on several key factors. These include the underlying cause of the mass, its stage or extent, and the patient’s overall health and preferences.
This section explores the various treatment modalities commonly employed. It underscores the importance of tailoring these options to meet the unique circumstances of each individual.
Tailoring Treatment to the Underlying Cause
The foundation of effective treatment lies in accurately identifying the etiology of the tissue mass. A benign condition will necessitate a vastly different approach than a malignant one.
-
Benign Conditions:
For benign conditions like Benign Prostatic Hyperplasia (BPH), treatment might focus on symptom management. This could involve medications to relax the prostate muscles or shrink the prostate gland. Minimally invasive procedures, such as transurethral resection of the prostate (TURP), might also be considered to alleviate urinary obstruction.
For prostatitis, treatment typically involves antibiotics to combat infection, along with supportive measures like pain management and lifestyle modifications.
-
Malignant Conditions:
When cancer is the underlying cause, treatment becomes more complex. A multidisciplinary approach is essential. This often involves a combination of surgery, radiation therapy, chemotherapy, and targeted therapies. The specific approach will depend on the type and stage of cancer, as well as the patient’s overall health.
Modalities of Treatment
Several treatment modalities are available, each with its own advantages and disadvantages.
-
Surgery:
Surgical intervention may be necessary to remove the tissue mass, particularly in cases of localized cancer. The type of surgery will depend on the location and extent of the mass. Radical prostatectomy, for example, is a common surgical approach for prostate cancer. Surgical removal can be curative if the cancer is localized.
-
Radiation Therapy:
Radiation therapy uses high-energy rays to kill cancer cells. It can be delivered externally using machines or internally using radioactive seeds implanted near the tumor (brachytherapy). Radiation therapy can be used as a primary treatment or as an adjuvant therapy after surgery.
-
Chemotherapy:
Chemotherapy involves the use of drugs to kill cancer cells throughout the body. It is often used for cancers that have spread beyond the pelvis. Chemotherapy can have significant side effects, so it’s typically reserved for more advanced stages of cancer.
-
Medication:
Medications play a crucial role in managing tissue masses. As stated before, they can manage BPH symptoms. Hormone therapy can be used to treat prostate cancer by lowering testosterone levels.
The Role of the Urologist
The urologist is a key figure in the treatment of tissue masses in the male pelvis. They are specialists in the urinary tract and male reproductive organs.
They are often the first point of contact for patients experiencing symptoms.
The urologist is responsible for:
- Diagnosis: Performing the initial evaluation and ordering the necessary diagnostic tests.
- Treatment Planning: Developing a personalized treatment plan in consultation with other specialists.
- Surgical Intervention: Performing surgical procedures to remove the tissue mass.
- Ongoing Management: Monitoring the patient’s progress and managing any side effects of treatment.
Effective management of tissue masses in the male pelvis requires a coordinated effort. The urologist will work closely with other specialists. These specialists can include oncologists, radiation oncologists, and pathologists. This multidisciplinary approach ensures that the patient receives the most comprehensive and effective care possible.
The Care Team: Navigating the Expertise Behind Your Treatment
The journey of diagnosing and treating a tissue mass in the male pelvis often involves a team of highly specialized medical professionals. Understanding the roles of each specialist is crucial for patients and their families.
This understanding allows for better communication, informed decision-making, and a greater sense of control throughout the treatment process.
Here, we will explore the key specialists you may encounter, highlighting their distinct expertise and contributions to your care.
The Urologist: Guardian of the Urinary and Male Reproductive Systems
The urologist is often the primary point of contact for men experiencing pelvic symptoms. They are specialists in the diagnosis and treatment of conditions affecting the urinary tract and male reproductive organs.
This includes the kidneys, bladder, ureters, urethra, prostate gland, and testes.
Key Responsibilities of the Urologist
- Diagnosis: Urologists are skilled in identifying the cause of your symptoms. They use a variety of diagnostic tools, including physical exams, imaging studies (such as ultrasounds, CT scans, and MRIs), and cystoscopies.
- Treatment of Benign Conditions: For benign conditions like BPH or prostatitis, urologists provide medical management. This includes prescribing medications to alleviate symptoms and performing minimally invasive procedures to improve urinary flow.
- Surgical Intervention: Urologists are surgeons who perform procedures to remove or treat tissue masses. This could involve prostatectomies for prostate cancer or TURP for BPH.
- Collaboration: Urologists work closely with other specialists. These specialists are oncologists, radiation oncologists, and pathologists, to coordinate the best possible care.
The urologist’s comprehensive knowledge of the male pelvic anatomy and related conditions makes them a central figure in your care team.
The Oncologist: Cancer Management and Systemic Therapies
When a tissue mass is identified as cancerous, an oncologist becomes a crucial member of the care team.
Oncologists are specialists in the diagnosis and treatment of cancer. They oversee systemic therapies, aiming to eradicate cancer cells throughout the body.
Oncologists and Their Critical Role in Treatment
- Diagnosis and Staging: Oncologists determine the type and stage of cancer. They assess how far it has spread, using sophisticated imaging and pathological data.
- Systemic Treatment Planning: They develop personalized treatment plans. The plans encompass chemotherapy, hormone therapy, targeted therapy, and immunotherapy.
- Chemotherapy Administration: Oncologists oversee the administration of chemotherapy. The chemotherapy utilizes powerful drugs to kill cancer cells.
- Hormone Therapy Management: For hormone-sensitive cancers like prostate cancer, oncologists manage hormone therapy. Hormone therapy aims to block the effects of hormones that fuel cancer growth.
- Immunotherapy Oversight: Oncologists administer immunotherapies that boost the body’s own immune system to fight cancer.
- Collaboration: Oncologists collaborate with surgeons and radiation oncologists to coordinate comprehensive cancer care.
- Palliative Care: Oncologists play a key role in palliative care, focusing on symptom management and improving quality of life for patients with advanced cancer.
The oncologist’s expertise in cancer biology and systemic therapies is vital for effective cancer management.
The Pathologist: Unveiling the Nature of the Mass
The pathologist is a medical doctor who specializes in diagnosing diseases. The diagnosis is done by examining tissues and fluids under a microscope.
Their role is essential in determining whether a tissue mass is benign or malignant. They also identify the specific type of cancer.
The Pathologist’s Diagnostic Precision
- Tissue Analysis: Pathologists analyze tissue samples obtained through biopsies or surgical resections.
- Microscopic Examination: They examine cells under a microscope to identify abnormalities. This includes cancer cells, inflammation, or other signs of disease.
- Diagnosis Confirmation: Pathologists provide a definitive diagnosis. This helps to determine the nature of the mass (benign or malignant). They also identify the specific type and grade of cancer, if present.
- Prognostic Information: Pathologists provide information about the likely course of the disease. This can include assessing the aggressiveness of the cancer and predicting its response to treatment.
- Collaboration: Pathologists work closely with surgeons and oncologists to ensure accurate diagnoses. The diagnoses are crucial for guiding treatment decisions.
The pathologist’s diagnostic precision is fundamental to guiding the entire treatment strategy. Their work provides the foundation upon which all other treatment decisions are made.
Understanding the specific roles of these medical specialists will empower you to navigate your care with confidence. Knowing who to ask, and what they specialize in, ensures you are actively involved in your healthcare decisions.
FAQs: Understanding Tissue Mass in the Male Pelvis
Here are some frequently asked questions to help you better understand what a tissue mass in the male pelvis might mean.
What exactly is a tissue mass in the male pelvis?
A tissue mass in the male pelvis simply refers to an abnormal growth of cells or tissue located within the pelvic region of a male. This tissue mass pelvis male can be benign (non-cancerous) or malignant (cancerous). Further investigation is needed to determine the precise nature of the mass.
What are some potential causes of a tissue mass pelvis male?
Several factors can cause a tissue mass in the pelvis of a male. These can include benign growths like cysts or polyps, inflammatory conditions, or, more seriously, various types of cancer affecting the prostate, bladder, rectum, or other pelvic organs. The precise cause often requires medical imaging and potentially a biopsy.
How is a tissue mass pelvis male typically diagnosed?
Diagnosis usually involves a physical exam, a review of medical history, and imaging tests such as an ultrasound, CT scan, or MRI. If a mass is detected, a biopsy might be performed to analyze the tissue and determine whether it is cancerous.
What are the common treatment options for a tissue mass pelvis male?
Treatment depends entirely on the diagnosis. Benign masses may only require monitoring. Cancerous masses might require surgery, radiation therapy, chemotherapy, or a combination of these approaches. Discuss treatment options with your doctor to understand the best course of action based on your specific situation.
So, that’s the lowdown on tissue mass pelvis male! Hopefully, this gave you a clearer picture. If anything seems off, chat with your doctor – they’re the real experts. Stay healthy!