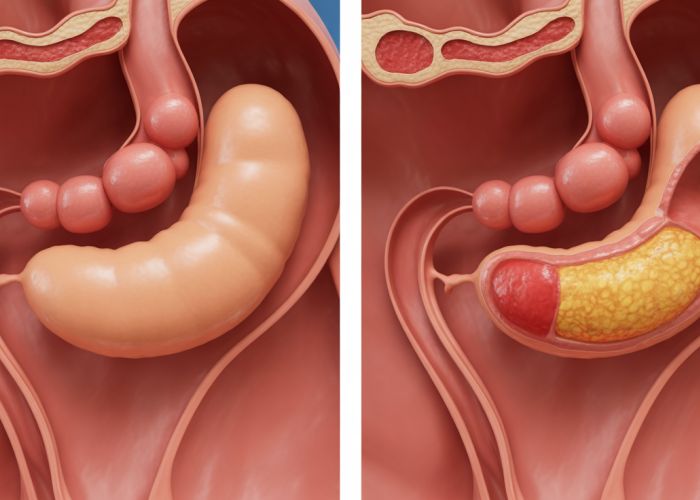
Understanding abdominal pain can be incredibly stressful, especially when differentiating between conditions with overlapping symptoms. Pelvic Inflammatory Disease (PID), a serious infection of the female reproductive organs, shares some symptoms with both ovarian issues and appendicitis, making accurate diagnosis crucial. The Mayo Clinic emphasizes the importance of prompt medical evaluation to rule out serious causes. Often, diagnostic imaging, such as an ultrasound, is used by healthcare professionals to differentiate between these conditions. Indeed, early intervention by a skilled gynecologist or emergency room physician is paramount. Navigating the complexities of abdominal pain and determining whether it’s related to your ovary or empendicities requires careful consideration and expert medical guidance. Hopefully, this article helps provide some insights!
Understanding the Difference: Ovary Pain vs. Appendicitis
Differentiating between ovary pain and appendicitis can be tricky because both conditions can cause lower abdominal pain. However, understanding the distinct characteristics of each will help you recognize potential symptoms and seek appropriate medical attention. Let’s explore the telltale signs to help you distinguish "ovary or appendicitis".
The Location and Nature of Pain
The location and quality of pain are crucial in distinguishing between these two conditions.
Ovary Pain
Ovary pain is typically located in the lower abdomen, either on the left or right side, depending on which ovary is affected. The pain can be:
- Sharp and stabbing: This type of pain is often associated with ovulation or a ruptured ovarian cyst.
- Dull and achy: This pain may indicate a more chronic issue, such as endometriosis or pelvic inflammatory disease (PID).
- Cyclical: Pain that coincides with your menstrual cycle is highly indicative of an ovarian issue.
It’s essential to consider the menstrual cycle as a significant factor. Pain related to ovulation (mittelschmerz) typically occurs mid-cycle and is brief. Pain associated with menstruation can vary in intensity and duration.
Appendicitis
Appendicitis, on the other hand, usually starts with pain around the navel (belly button) that gradually migrates to the lower right abdomen. This is a hallmark sign. The pain associated with appendicitis is often:
- Constant and worsening: Unlike ovary pain which can fluctuate, appendicitis pain generally becomes progressively more severe.
- Sharp and intense: It’s often described as a sharp, localized pain in the lower right abdomen.
- Aggravated by movement: Coughing, sneezing, or even walking can exacerbate the pain.
Associated Symptoms
Beyond the location of pain, additional symptoms can help pinpoint the source of the discomfort.
Symptoms Suggestive of Ovary Issues
Here are some symptoms that could signal a problem with your ovaries:
- Irregular periods: Changes in your menstrual cycle, such as skipped periods, heavier bleeding, or spotting, may indicate an ovarian issue.
- Bloating: Persistent bloating or a feeling of fullness in the abdomen.
- Nausea and vomiting: These can accompany ovary pain, especially during ovulation or if there’s a cyst rupture.
- Pain during intercourse: This symptom, known as dyspareunia, can be associated with endometriosis or other ovarian conditions.
- Changes in bowel or bladder habits: These are less common but can occur.
Symptoms Suggestive of Appendicitis
Consider these symptoms that commonly present with appendicitis:
- Fever: A low-grade fever (around 100-101°F or 37.7-38.3°C) is common.
- Loss of appetite: A noticeable decrease in appetite or feeling unable to eat.
- Nausea and vomiting: These are often present and may occur before the pain fully localizes to the lower right abdomen.
- Constipation or diarrhea: Changes in bowel habits can occur but are not always present.
- Abdominal tenderness: When a doctor presses on your lower right abdomen, it will be extremely tender. This is a key diagnostic sign.
Risk Factors and Medical History
Certain factors can increase the likelihood of either condition, providing further clues.
Risk Factors Related to Ovary Problems
Consider the following when evaluating the possibility of ovary-related pain:
- Age: Women of reproductive age are more susceptible to ovarian cysts, endometriosis, and other ovarian conditions.
- Medical history: A history of ovarian cysts, endometriosis, or pelvic inflammatory disease (PID) increases your risk of recurrent ovarian pain.
- Family history: A family history of ovarian cancer or endometriosis might raise concerns.
Risk Factors Related to Appendicitis
While appendicitis can affect anyone, here are some factors to keep in mind:
- Age: Appendicitis is most common in people between the ages of 10 and 30.
- Family history: While less significant than with ovary problems, a family history of appendicitis might slightly increase your risk.
- Other medical conditions: Though rare, certain medical conditions can increase the risk of appendicitis.
A Quick Reference Table
Here is a simple table summarizing the key differences:
| Feature | Ovary Pain | Appendicitis |
|---|---|---|
| Pain Location | Lower abdomen (left or right) | Starts around navel, moves to lower right |
| Pain Quality | Sharp, dull, cyclical | Constant, worsening, sharp |
| Fever | Uncommon, or low-grade | Common (low-grade) |
| Appetite | May be affected, but not always severely | Significant loss of appetite |
| Menstrual Cycle | Relevant, may coincide with pain | Irrelevant |
| Movement | May or may not affect pain | Aggravates pain |
When to Seek Medical Attention
It is crucial to seek medical attention if you experience:
- Severe abdominal pain: Pain that is unbearable or rapidly worsening.
- High fever: A fever above 101°F (38.3°C).
- Persistent vomiting: Inability to keep down fluids.
- Signs of shock: Rapid heart rate, shallow breathing, dizziness.
- Uncertainty: If you are unsure about the cause of your abdominal pain, it is always best to consult a healthcare professional for an accurate diagnosis and appropriate treatment. Do not hesitate; early diagnosis is vital for both appendicitis and serious ovary issues. A medical professional can conduct a physical exam, review your medical history, and order diagnostic tests (such as blood tests, urine tests, ultrasound, or CT scans) to determine the underlying cause of your pain.
Ovary vs. Appendicitis: Frequently Asked Questions
Here are some common questions about differentiating between ovary pain and appendicitis. Understanding the nuances can help you seek timely and appropriate medical attention.
Can ovary pain feel similar to appendicitis?
Yes, pain from ovary-related issues, especially on the right side, can sometimes mimic appendicitis. Both conditions can cause lower abdominal pain. It’s crucial to consider other symptoms for an accurate diagnosis.
What symptoms are more indicative of appendicitis over ovary problems?
While both can cause nausea and pain, appendicitis is more likely to cause fever and a sharp, localized pain that worsens quickly. Ovary problems may cause pain related to your menstrual cycle. The only sure way is to have a medical professional test you.
How can a doctor tell the difference between pain from the ovary or appendicitis?
Doctors use a combination of physical exams, symptom evaluation, and diagnostic tests like blood tests, urine tests, and imaging (CT scan or ultrasound). These tests help pinpoint the source of the pain and rule out other possibilities.
Is it possible to have both ovary issues and appendicitis simultaneously?
While rare, it is possible to experience both ovary issues and appendicitis at the same time. This can make diagnosis more challenging, highlighting the importance of a thorough medical evaluation. If you are unsure about where the pain is coming from, contact your doctor immediately.
Alright, that covers the essentials on understanding the difference between potential ovary and empendicities issues! Remember, I’m not a doctor, so this isn’t medical advice. If you’re feeling any funky pain, please go get checked out by a pro – better safe than sorry!